For decades, common table salt has been cast as a major villain in the narrative of cardiovascular health. People interested in personal health and the like have avoided it. Today health professionals and dietary guidelines are cautioning against its excessive consumption. This is due mainly to the belief that it directly contributes to heart disease, hypertension, and stroke.
The conventional wisdom held that salt, or more specifically, the sodium it contains, was a primary culprit in raising blood pressure. This in turn is a significant risk factor for cardiovascular disease and something to be avoided by health conscious people. This stance led to widespread efforts to minimize salt intake as a preventative measure against heart-related conditions.
Historically, the relationship between salt and heart health was seen as straightforward. High salt intake was thought to increase blood pressure, which in turn, raised the risk of heart disease. This commonly held belief was supported by numerous studies and health organizations worldwide. They in turn advocated for reduced sodium diets as part of a heart-healthy lifestyle. Public health campaigns and dietary guidelines reflected this stance. It was common to hear them urging people to limit their consumption of salt-rich foods. People were warned about the dangers of the sodium content in processed foods and restaurant meals.
No One Size Fits All
However, as we shall see, recent research has begun to paint a more complex picture of the role of salt in cardiovascular health. Studies emerging in the last decade have challenged the one-size-fits-all approach to salt consumption. They are now suggesting that the impact of salt on heart health may not be nearly as detrimental for everyone as previously thought. These studies indicate that the relationship between salt intake and heart disease is more nuanced. It depends more on individual differences in salt sensitivity, genetic factors, and overall dietary patterns to name just a few variables.
One pivotal area of new research focuses on the concept of salt sensitivity. This sensitivity refers to the variation in how individuals’ blood pressure responds to salt intake. Some people experience significant increases in blood pressure with higher salt consumption. Others people however, show little to no change (salt-resistant individuals). This variability suggests that blanket recommendations for salt intake might not be appropriate for everyone. Again underscoring the need for personalized dietary advice based on individual health profiles and genetic predispositions.
Salt Studies
Recent studies have also explored the potential benefits of salt in the diet. Salt plays a crucial role in bodily functions. They include fluid balance, nerve transmission, and muscle contraction. It is also an essential electrolyte that helps with hydration and cardiovascular function. The nuanced view acknowledges that while excessive salt intake can be harmful. This is especially so for those with hypertension or pre-existing heart conditions. Moderate consumption within a balanced diet however, might not pose the same level of risk for healthy individuals.
The evolving perspective on salt and heart health is also prompting a reevaluation of how dietary guidelines are formulated. Instead of strict limits on salt intake for the entire population, some researchers are advocating for guidelines. These guidelines take into consideration the complexity of individual health needs and the overall dietary context. For example, the quality of the diet as a whole—rich in fruits, vegetables, whole grains, and lean proteins—may mitigate the potential negative effects of a higher salt intake.
A More Nuanced Approach
This shift towards a more nuanced understanding of salt’s impact on heart health emphasizes the importance of considering individual differences, the role of other dietary factors, and the balance of risks and benefits when making dietary recommendations. It reflects a broader trend in nutrition science towards personalized nutrition and the recognition that dietary advice must be adaptable to meet the diverse needs of the population.

Debunking Myths About Salt and Heart Health
The common narrative around salt and its effects on heart health has been a point of contention and misunderstanding within both the medical community and public perception for decades on end. Historically, salt has been labeled as harmful, primarily due to its association with high blood pressure, a well known risk factor for heart disease and stroke.
This belief and ubiquitous perspective was largely influenced by early observational studies and clinical trials that showed a reduction in blood pressure following a decrease in salt intake. As a result, dietary guidelines worldwide have recommended low-sodium diets as a universal strategy for reducing heart disease risk.
Historical Context of Salt’s Harmful Label
The view of salt consumption being a bad thing began taking shape in the latter half of the 20th century when researchers first started linking high sodium intake with elevated blood pressure. Public health policies were subsequently influenced by these findings, leading to the widespread promotion of salt-reduction strategies to combat heart disease and a heck of a lot of bad press for salt and sodium. The simplicity of the message – less salt equals better heart health – was appealing for its ease of understanding and implementation. However, this approach failed to account for individual variability and the complexity of dietary patterns contributing to cardiovascular health and is more “truthy” and truth.
Recent Research Challenges the Old Narrative
In recent years, a growing body of clinical research has begun to challenge the traditional dogma on salt. The idea that all individuals benefit from reducing salt intake is under attack. A seminal turning point came with the recent publication of studies. These studies are suggesting that the relationship between salt and heart health is not straightforward. For example, a series of articles published in the “New England Journal of Medicine” in 2014 highlighted the potential risks of both high and low sodium intake. These indicate and suggest a U-shaped relationship between salt consumption and health outcomes. This means that both excessive and insufficient salt intake could be associated with adverse health effects.
Moreover, the PURE (Prospective Urban Rural Epidemiology) study, one of the largest epidemiological studies to date, found that the association between sodium intake and cardiovascular events, as well as mortality, followed a J-shaped curve. This research indicated that while very high sodium intake was linked to increased heart disease risk, moderate intake was not, and very low intake might even be harmful.
Examples of Non-linear Relationship Studies
These findings underscore the complexity of the relationship between salt intake and heart disease risk. For instance, a meta-analysis published in the “Lancet” in 2016 analyzed data from over 130,000 individuals and concluded that low sodium intake was associated with an increased risk of cardiovascular events and death in individuals without hypertension. However this study has come under serious attack.
Conversely, only high sodium intake (exceeding 6 grams per day) was associated with an increased risk among those with high blood pressure.
Such evidence suggests a need to revisit and refine public health guidelines concerning salt consumption. Instead of a one-size-fits-all approach, there’s a growing consensus among scientists and nutrition experts for guidelines that consider individual health status, dietary context, and even genetic predispositions.
A Shift In Understanding
The shift in understanding underscores the importance of nuanced dietary advice and the need for continued research. We need to better identify those who may benefit from salt reduction . We also must identify those for whom too little salt may be just as concerning. This evolving narrative challenges long-standing dietary dogmas. It also opens the door for more personalized nutrition strategies that better reflect the complexities of human health.
Balancing Salt Intake for Optimal Heart Health
Achieving a balanced salt intake is crucial for maintaining heart health. Without unnecessarily restricting dietary pleasures, salt after all tastes good. Moderation and mindful consumption are key, alongside an understanding of how dietary quality and the source of salt can influence overall health outcomes.
Guidelines for Moderating Salt Consumption
- Understand Individual Needs: Recognize personal health factors, such as blood pressure levels and any history of heart disease, to tailor salt intake accordingly, you may or may not be sensitive to salt so some personal monitoring is advised.
- Aim for Moderation: The American Heart Association recommends no more than 2,300 milligrams a day, moving toward an ideal limit of about 1,500 mg per day for most adults.
The Role of Diet Quality and Salt Source
- Prioritize Whole Foods: Focus on fresh fruits, vegetables, whole grains, and lean proteins, which naturally contain lower amounts of sodium, while at the same time, not overdoing it on the sugars.
- Limit Processed Foods: These are the primary sources of high sodium in the diet, often containing much more salt than their natural or homemade counterparts, and are bad for you in so many other ways due to trans-fats and other ingredients.
- Choose Natural Salt Sources: When adding salt to foods, opt for unprocessed or minimally processed salts. Be mindful that all forms of salt have similar sodium content by weight, but natural sources may offer trace minerals.
Tips for Adding Flavor Without Excessive Salt
- Use Herbs and Spices: Enhance flavor with a variety of herbs, spices, citrus, vinegar, and garlic instead of relying solely on salt, there are many other flavors to choose from!
- Experiment with Salt-Free Seasoning Blends: Many blends can provide depth of flavor to dishes without adding sodium.
- Balance with Acidity: A splash of lemon juice or vinegar can brighten dishes, often reducing the need for added salt.
Practical Tips for Managing Salt Intake
Managing salt intake does not have to mean sacrificing flavor or enjoyment of food. By adopting some practical strategies, it’s possible to reduce sodium consumption while still enjoying a rich and varied diet.
Strategies for Reducing Reliance on Processed Foods
- Cook More at Home: Preparing meals from scratch gives you control over the amount of salt used.
- Choose Fresh or Frozen Produce: Opt for fresh or frozen fruits and vegetables, which are low in sodium, over canned varieties that may contain added salt.
- Select Low-Sodium Products: When buying processed foods, look for items labeled “low sodium,” “reduced sodium,” or “no salt added.”
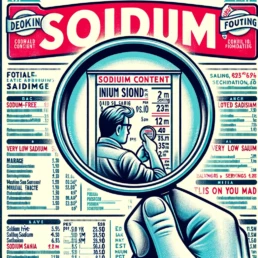
How to Read Food Labels for Better Sodium Management
- Check the Sodium Content: Pay attention to the milligrams of sodium per serving and the number of servings per package.
- Understand Sodium Descriptors: Learn what terms like “sodium-free,” “very low sodium,” and “low sodium” mean in terms of actual sodium content.
Incorporating Potassium-Rich Foods to Balance Sodium Intake
- Eat Potassium-Rich Foods: Foods high in potassium, such as bananas, potatoes, spinach, and beans, can help counteract the effects of sodium and support healthy blood pressure.
- Understand the Sodium-Potassium Balance: A diet high in potassium can help to mitigate some of the negative effects of high sodium intake on blood pressure.
By embracing these guidelines and tips, you can find a healthy balance in your salt intake that supports heart health without diminishing the joy of eating. This approach encourages a more holistic view of diet, focusing on overall nutritional balance and the quality of ingredients, rather than simply cutting out salt.